Healthcare Fraud Detection Market Size
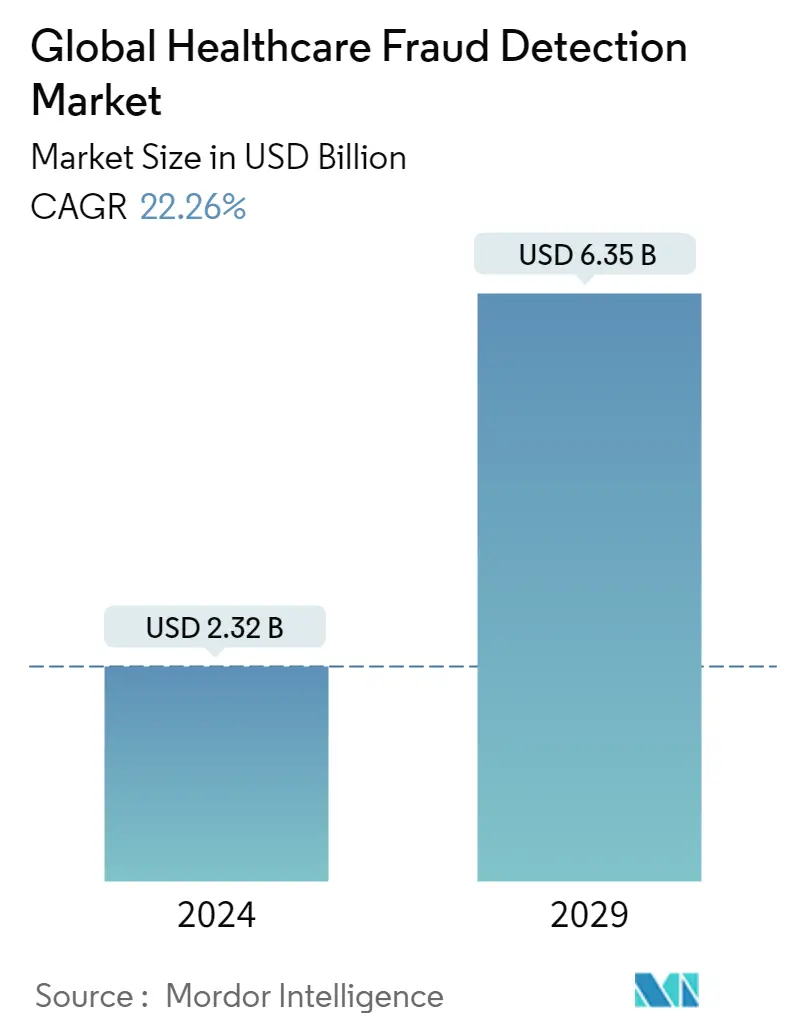
| Study Period | 2019 - 2029 |
| Market Size (2024) | USD 2.32 Billion |
| Market Size (2029) | USD 6.35 Billion |
| CAGR (2024 - 2029) | 22.26 % |
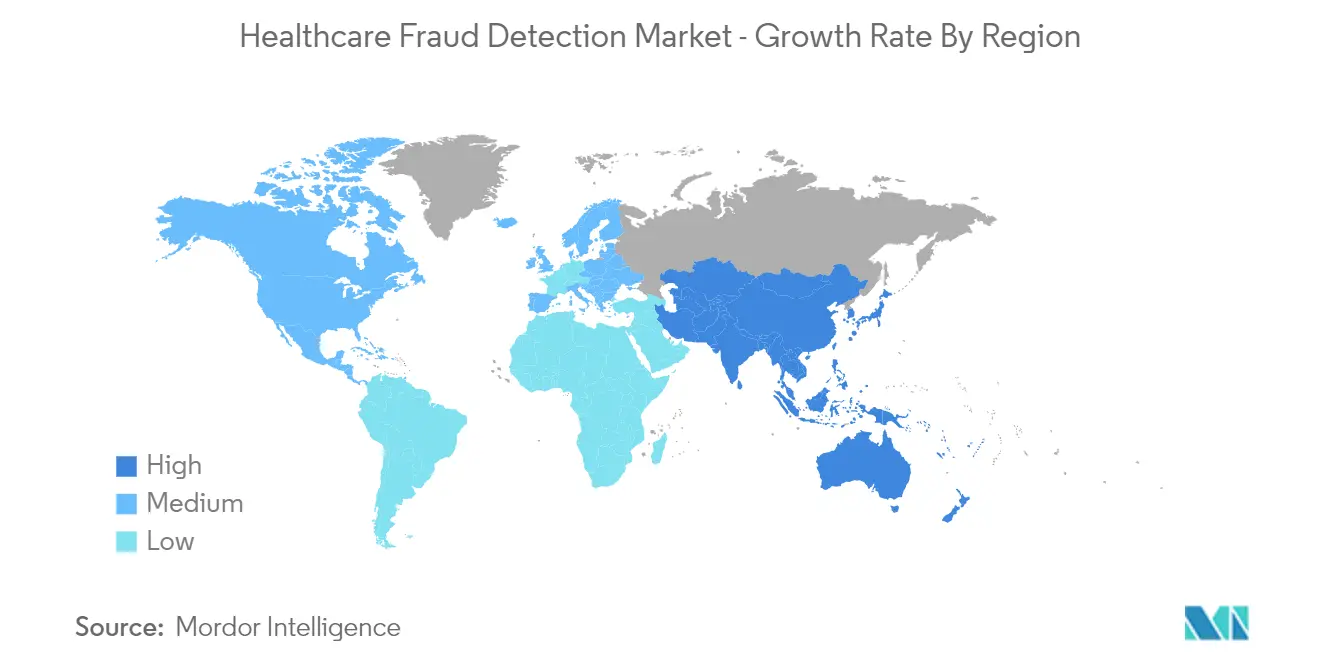
| Fastest Growing Market | Asia Pacific |
| Largest Market | North America |
Major Players
*Disclaimer: Major Players sorted in no particular order |
Healthcare Fraud Detection Market Analysis
The Global Healthcare Fraud Detection Market size is estimated at USD 2.32 billion in 2024, and is expected to reach USD 6.35 billion by 2029, growing at a CAGR of 22.26% during the forecast period (2024-2029).
Since the COVID-19 pandemic started, it has drastically affected the healthcare industry. While some markets in the industry have shown a downfall, some have shown increased growth. The healthcare industry has witnessed several fraud cases committed by patients, doctors, physicians, and other medical specialists. It was observed that many healthcare providers and specialists are engaged in fraudulent activities for profit. Many instances prove the increasing number of fraud cases during the pandemic. The Justice Department's False Claims Act Settlements and Judgments exceeded USD 5.6 billion in 2021, and it was the second-largest amount recorded since 2014, and of the amount settled, over USD 5 billion in matters related to the health care industry, which includes drug and medical device manufacturers, managed care providers, hospitals, pharmacies, hospice organizations, laboratories, and physicians, among others. Such factors boosted the adoption of healthcare fraud detection solutions, thereby driving the market's growth over the pandemic phase.
Furthermore, the major factors driving the growth of the market are the rising healthcare expenditure; the increasing number of patients opting for health insurance; growing pressure to increase operational efficiency and reduce healthcare spending, and surging fraudulent activities in the healthcare sector globally.
An increasing number of providers are billing and claiming federal health care programs for medically unnecessary services or services not rendered as billed. For instance, in May 2021, SavaSeniorCare LLC and its subsidiaries agreed to pay a settlement amount of USD 11.2 million for alleged false claims for rehabilitation therapy services that they provided because of aggressive corporate targets without respecting the patients' clinical needs. Likewise, Alere billed and caused others to charge for defective rapid point-of-care testing devices, which were used by Medicare beneficiaries to monitor blood coagulation when taking anticoagulant drugs, and for this, the company paid USD 38.75 million as a settlement as per the source mentioned above. These increasing fraudulent activities in the healthcare industry are increasing the demand for healthcare fraud detection services and solutions, which is positively affecting the growth of the market.
Additionally, in the upper-income countries, healthcare expenditure was observed to be equally distributed, resulting in the overall development of the healthcare system. On the contrary, people in the low- and middle-income countries have to pay from their own pockets due to less contribution from the governments toward healthcare expenditure which is resulting in more healthcare fraud, and this is proportionally increasing the demand for healthcare fraud detection solutions.
Thus, the market is expected to project growth over the forecast period. However, the lack of adoption of healthcare fraud analytics may hamper the growth of the market.
Healthcare Fraud Detection Market Trends
This section covers the major market trends shaping the Healthcare Fraud Detection Market according to our research experts:
Review of Insurance Claims by Application Segment is Expected to Witness Growth Over the Forecast Period
Healthcare Fraud Detection solutions play a major role in the review of insurance claims, as most fraud cases occur while claiming insurance. In healthcare insurance fraud, false information is provided to a health insurance company to have them pay unauthorized benefits to the policyholder or the service provider. Machine learning techniques help in improving predictive accuracy and enable loss control units to achieve higher coverage with low false-positive rates. Moreover, the quality and quantity of the available data have a huge impact on the predictive accuracy compared to the quality of the algorithm.
Globally, various organizations, such as the Insurance Fraud Bureau of Australia (IFBA), the Canadian Life and Health Insurance Association (CLHIA), the NHS Counter Fraud Authority (NHSCFA), and the European Healthcare Fraud & Corruption Network (EHFCN), among others, aim to reduce healthcare insurance fraud. The growing interest of the government and private sectors in the review of healthcare insurance claims to save individuals and nations money is driving the growth of the segment.
The Insurance Regulatory and Development Authority of India (IRDAI), annual report 2021, reported that, globally, the share of life insurance business in total premium was 44.5%, and the share of non-life insurance premium was 55.5% in 2020, but India's share of life insurance business was high, and it was at 75.24%, while non-life insurance for non-life business accounted for only 24.76%. This high number of health care life insurance claims has been increasing the demand for solutions in reviewing the insurance claim segment.
Therefore, the increasing number of insurance claims by patients, family members, companies, and others is increasing the demand for the review of the insurance claims segment over the forecast period.
North America Dominates the Market and is Expected to Do the Same over the Forecast Period
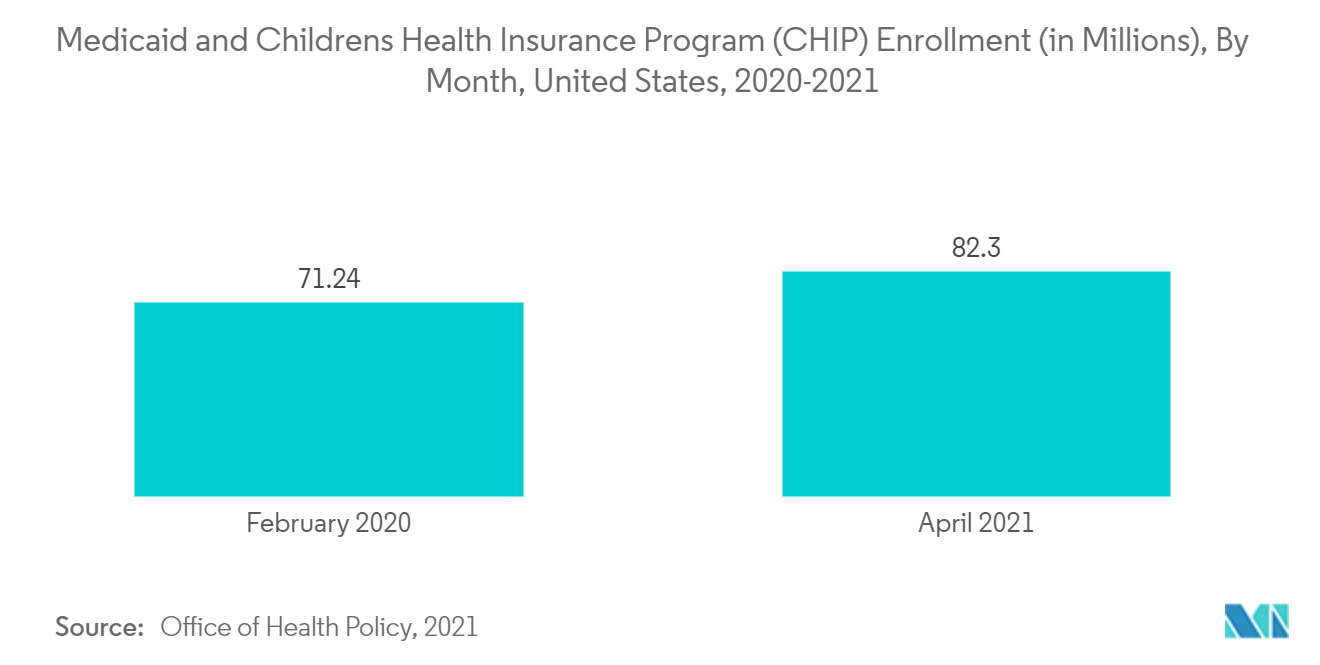
North America is expected to dominate the overall market throughout the forecast period. This is due to increasing healthcare spending, rising healthcare IT adoption, and the growing number of fraud cases in the healthcare industry.
The National Health Care Anti-Fraud Association (NHCAA) website Consumer Information section, updated in 2021, stated that every year the United States spends over USD 2.27 trillion on health care. An NHCAA estimate shows that USD 10 billion is lost to health care fraud, and USD 54 billion is estimated to be scammed and stolen every year in the United States. These activities and the loss of wealth in the form of fraud and illegal activities make healthcare fraud the biggest problem in the country. This is expected to drive the demand for healthcare fraud detection solutions over the forecast period.
Additionally, in June 2021, Artivatic launched the ALFRED-AI HEALTH CLAIMS platform for automating end-to-end health claims, and its fraud and abuse detection capacity is 30% or more. The ALFRED-AI HEALTH CLAIMS platform also allows users to self-learn and evolve a system for better risk assessment, fraud detection, and decision-making.
Thus, owing to the availability of numerous advanced services and solutions related to healthcare fraud detection and strategic steps taken by major players present in the country, the market for healthcare fraud detection is expected to bolster within the North American region.
Healthcare Fraud Detection Industry Overview
The Healthcare Fraud Detection market is moderately competitive and consists of several major players. In terms of shares, a few of the major players currently dominate the market. With the rising adoption of healthcare IT and the increasing number of fraud cases, a few other smaller players are expected to enter the market in the coming years. Some of the major players in the market are CGI Inc., DXC Technology Company, ExlService Holdings, Inc. (Scio Health Analytics), International Business Machines Corporation (IBM), McKesson Corporation, Northrop Grumman, OSP Labs, SAS Institute Inc., RELX Group plc, and UnitedHealth Group (Optum Inc.), among others.
Healthcare Fraud Detection Market Leaders
-
CGI Inc.
-
DXC Technology Company
-
International Business Machines Corporation (IBM)
-
Mckesson
-
ExlService Holdings, Inc.
*Disclaimer: Major Players sorted in no particular order
Healthcare Fraud Detection Market News
- In March 2022, Veriff released a new suite of biometrics-powered identity verification solutions designed specifically for the healthcare industry. According to the company, the new offering will utilize artificial intelligence and facial recognition technologies to perform user identification.
- In February 2022, the Canadian Life and Health Insurance Association (CLHIA) launched an industry initiative to pool claims data and use advanced artificial intelligence tools to enhance the detection and investigation of benefits fraud.
Healthcare Fraud Detection Market Report - Table of Contents
1. INTRODUCTION
- 1.1 Study Assumptions and Market Definition
- 1.2 Scope of the Study
2. RESEARCH METHODOLOGY
3. EXECUTIVE SUMMARY
4. MARKET DYNAMICS
- 4.1 Market Overview
-
4.2 Market Drivers
- 4.2.1 Rising Healthcare Expenditure
- 4.2.2 Rise in the Number of Patients Opting for Health Insurance
- 4.2.3 Growing Pressure to Increase Operational Efficiency and Reduce Healthcare Spending
- 4.2.4 Increasing Fraudulent Activities in Healthcare
-
4.3 Market Restraints
- 4.3.1 Unwillingness to Adopt Healthcare Fraud Analytics
-
4.4 Porter's Five Forces Analysis
- 4.4.1 Threat of New Entrants
- 4.4.2 Bargaining Power of Buyers/Consumers
- 4.4.3 Bargaining Power of Suppliers
- 4.4.4 Threat of Substitute Products
- 4.4.5 Intensity of Competitive Rivalry
5. MARKET SEGMENTATION (Market Size by Value - USD million)
-
5.1 By Type
- 5.1.1 Descriptive Analytics
- 5.1.2 Predictive Analytics
- 5.1.3 Prescriptive Analytics
-
5.2 By Application
- 5.2.1 Review of Insurance Claims
- 5.2.2 Payment Integrity
-
5.3 End User
- 5.3.1 Private Insurance Payers
- 5.3.2 Government Agencies
- 5.3.3 Other End Users
-
5.4 Geography
- 5.4.1 North America
- 5.4.1.1 United States
- 5.4.1.2 Canada
- 5.4.1.3 Mexico
- 5.4.2 Europe
- 5.4.2.1 Germany
- 5.4.2.2 United Kingdom
- 5.4.2.3 France
- 5.4.2.4 Italy
- 5.4.2.5 Spain
- 5.4.2.6 Rest of Europe
- 5.4.3 Asia-Pacific
- 5.4.3.1 China
- 5.4.3.2 Japan
- 5.4.3.3 India
- 5.4.3.4 Australia
- 5.4.3.5 South Korea
- 5.4.3.6 Rest of Asia-Pacific
- 5.4.4 Middle East and Africa
- 5.4.4.1 GCC
- 5.4.4.2 South Africa
- 5.4.4.3 Rest of Middle East and Africa
- 5.4.5 South America
- 5.4.5.1 Brazil
- 5.4.5.2 Argentina
- 5.4.5.3 Rest of South America
6. COMPANY PROFILES AND COMPETITIVE LANDSCAPE
-
6.1 Company Profiles
- 6.1.1 CGI Inc.
- 6.1.2 DXC Technology Company
- 6.1.3 ExlService Holdings, Inc.
- 6.1.4 International Business Machines Corporation (IBM)
- 6.1.5 McKesson Corporation
- 6.1.6 Northrop Grumman
- 6.1.7 OSP Labs
- 6.1.8 SAS Institute Inc.
- 6.1.9 RELX Group plc
- 6.1.10 UnitedHealth Group. (Optum Inc.)
- *List Not Exhaustive
7. MARKET OPPORTUNITIES AND FUTURE TRENDS
** Subject To AvailablityHealthcare Fraud Detection Industry Segmentation
As per the scope of the report, the term 'healthcare fraud detection' refers to solutions that are helpful in the early detection of errors in claim submissions, duplication of claims, etc., to minimize healthcare spending and improve efficiency. The healthcare fraud detection market is segmented by Type (Descriptive Analytics, Predictive Analytics, and Prescriptive Analytics), Application (Review of Insurance Claims and Payment Integrity), End User (Private Insurance Payers, Government Agencies, and Other End Users), and Geography (North America, Europe, Asia-Pacific, Middle East and Africa, and South America). The market report also covers the estimated market sizes and trends for 17 different countries across major regions globally. The report offers the value (in USD million) for the above segments.
| By Type | Descriptive Analytics | |
| Predictive Analytics | ||
| Prescriptive Analytics | ||
| By Application | Review of Insurance Claims | |
| Payment Integrity | ||
| End User | Private Insurance Payers | |
| Government Agencies | ||
| Other End Users | ||
| Geography | North America | United States |
| Canada | ||
| Mexico | ||
| Geography | Europe | Germany |
| United Kingdom | ||
| France | ||
| Italy | ||
| Spain | ||
| Rest of Europe | ||
| Geography | Asia-Pacific | China |
| Japan | ||
| India | ||
| Australia | ||
| South Korea | ||
| Rest of Asia-Pacific | ||
| Geography | Middle East and Africa | GCC |
| South Africa | ||
| Rest of Middle East and Africa | ||
| Geography | South America | Brazil |
| Argentina | ||
| Rest of South America |
Healthcare Fraud Detection Market Research FAQs
How big is the Global Healthcare Fraud Detection Market?
The Global Healthcare Fraud Detection Market size is expected to reach USD 2.32 billion in 2024 and grow at a CAGR of 22.26% to reach USD 6.35 billion by 2029.
What is the current Global Healthcare Fraud Detection Market size?
In 2024, the Global Healthcare Fraud Detection Market size is expected to reach USD 2.32 billion.
Who are the key players in Global Healthcare Fraud Detection Market?
CGI Inc., DXC Technology Company, International Business Machines Corporation (IBM), Mckesson and ExlService Holdings, Inc. are the major companies operating in the Global Healthcare Fraud Detection Market.
Which is the fastest growing region in Global Healthcare Fraud Detection Market?
Asia Pacific is estimated to grow at the highest CAGR over the forecast period (2024-2029).
Which region has the biggest share in Global Healthcare Fraud Detection Market?
In 2024, the North America accounts for the largest market share in Global Healthcare Fraud Detection Market.
What years does this Global Healthcare Fraud Detection Market cover, and what was the market size in 2023?
In 2023, the Global Healthcare Fraud Detection Market size was estimated at USD 1.90 billion. The report covers the Global Healthcare Fraud Detection Market historical market size for years: 2019, 2020, 2021, 2022 and 2023. The report also forecasts the Global Healthcare Fraud Detection Market size for years: 2024, 2025, 2026, 2027, 2028 and 2029.
Healthcare Fraud Detection Software Industry Report
Statistics for the 2024 Healthcare Fraud Detection Software market share, size and revenue growth rate, created by Mordor Intelligence™ Industry Reports. Healthcare Fraud Detection Software analysis includes a market forecast outlook to 2029 and historical overview. Get a sample of this industry analysis as a free report PDF download.