Healthcare Provider Network Management Market Size
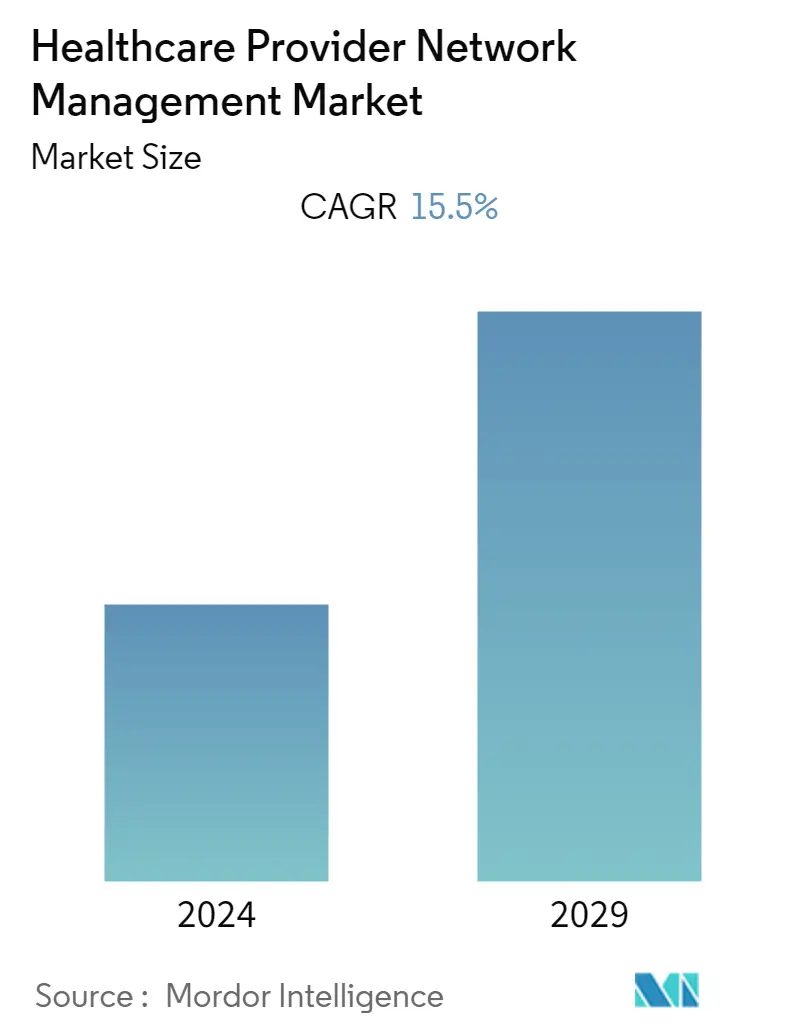
| Study Period | 2020 - 2029 |
| Base Year For Estimation | 2023 |
| CAGR | 15.50 % |
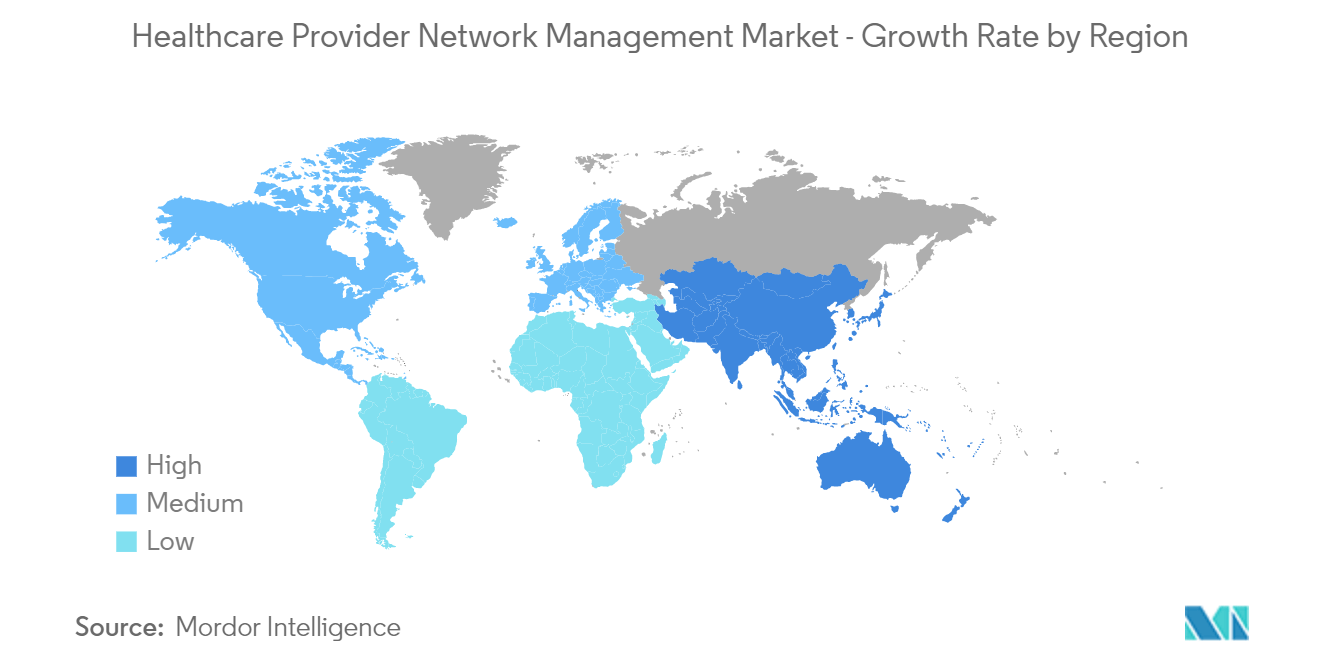
| Fastest Growing Market | Asia Pacific |
| Largest Market | North America |
| Market Concentration | High |
Major Players
*Disclaimer: Major Players sorted in no particular order |
Healthcare Provider Network Management Market Analysis
- The healthcare provider network management market is expected to witness a CAGR of 15.5% over the forecast period.
- The COVID-19 pandemic significantly impacted market growth, particularly in the healthcare sector. Healthcare provider management solutions have emerged as a useful tool in automating various processes, thus saving time and expenses. For example, a National Academy of Medicine (NAM) Perspectives article reported that healthcare insurance providers adopted a provider network management solution due to the increase in operating expenses resulting from the growing volume of COVID-19 patients and deferred health services. This solution helped manage claims with greater accuracy of provider networks, lower costs, and less burden on providers. As healthcare providers increasingly adopt provider network management solutions, the market has seen significant growth and is expected to continue growing over the forecast period.
- Several factors are expected to boost market growth, such as the rising quality of care through payer reporting requirements, increasing technological advancements related to healthcare IT solutions, and growing awareness about insurance policies. The rising number of people using insurance to deal with medical costs, such as treatment, hospitalization, and health check-ups, further fuels the demand for provider network management payer services, which is anticipated to drive market growth.
- The India Brand Equity Foundation (IBEF) published its Insurance Industry Report in November 2022, which showed an increase in the number of people who purchased insurance policies. The gross first-year premiums of life insurers increased by 6.94%, totaling INR 2,27,188 crore (USD 29.54 billion) in 2021-2022 (until 31st January 2022). The report also indicated that the new business premiums of life insurers had increased by 88.64% to INR 24,480.36 crore (USD 3.12 billion) in May 2021.
- Additionally, the emergence of technologically advanced solutions and systems in healthcare IT is expected to increase the adoption of provider network management solutions, thereby bolstering market growth. For example, TidalHealth partnered with Regard, an artificial intelligence (AI) software startup, in August 2022 to improve patient diagnostic accuracy, minimize physician exhaustion, and increase income through improved documentation. Modulim launched a software solution in November 2022 designed to empower clinicians with remote access to data insights and scalability to enhance clinical workflow across enterprises.
- Digital technologies also aid in the skillful management of large amounts of data, encourage value addition to the organization, and streamline compliance activities, assisting businesses in avoiding unintended, unanticipated outcomes. By using technology for data integration, analytics, and visualization, compliance activities are being digitized to enhance comprehension. It also helps prevent adverse events by employing robotic process automation and other cognitive technologies such as machine learning and artificial intelligence. These benefits are expected to increase the adoption of provider network management systems and platforms, propelling the market growth.
- Furthermore, the increasing company activities in developing advanced software and solutions are contributing to market growth. Optum launched Optum Specialty Fusion, a specialty medication management solution, in February 2022 to simplify care for patients with complex conditions and lower the cost of expensive specialty drugs.
- Specialized Fusion offers payers and providers real-time healthcare insight into the most efficient specialty treatments at the patient's lowest cost using Optum's data and clinical experience. Innovaccer launched Provider Network Management Solutions in March 2021 to assist healthcare payers in accessing a complete view and exercising control over their provider network performance. The solution creates a unified pool of accurate provider data, determines effective methods, incentivizes providers, and streamlines communication.
- Despite the expected growth of the studied market, some factors may impede market growth over the forecast period. The high cost of software installation and maintenance, as well as data security issues and cyberattacks, are likely to be barriers.
Healthcare Provider Network Management Market Trends
Cloud-based Delivery Segment is Expected to Witness Significant Growth Over the Forecast Period
- The healthcare provider network management market is expected to witness significant growth in the cloud-based delivery mode segment during the forecast period. This growth can be attributed to several factors, including the high number of cloud-based software and services available in the market and the increasing use of these technologies by healthcare providers.
- According to an article published in Korea Science in March 2021, cloud service providers offer a wide range of services that allow for the secure ingestion, storage, and processing of healthcare data. In addition, the cloud provides mid-sized hospitals with cost-effective solutions for administering their services, with strong computing, effective storage, and advanced analytics on healthcare data. The benefits offered by cloud-based software are expected to increase their adoption by healthcare providers, thereby boosting segment growth.
- Moreover, the increasing company activities in developing technologically advanced software and solutions are also expected to drive market growth. For instance, in October 2022, Innovaccer, the Health Cloud company, launched Innovaccer Health Limited, which accelerates innovation and digital transformation by offering Innovaccer's industry-leading Health Cloud, Data Activation Platform, and Healthcare Technology solutions.
- Additionally, in June 2021, Salesforce launched new artificial intelligence tools for its healthcare cloud platform to help providers better manage patient engagement and scheduling. Salesforce's Intelligent Appointment Management for Health Cloud integrates with electronic health records to find and reserve appointments for patients with their preferred doctors.
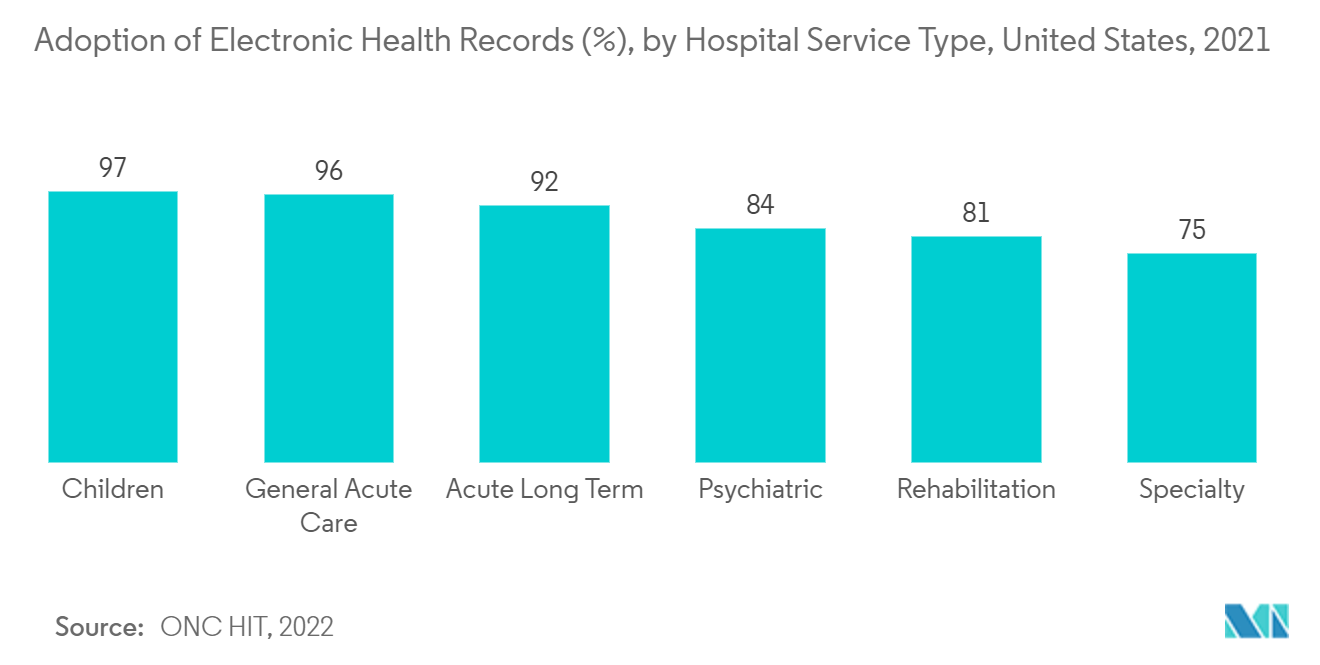
- Therefore, the adoption of cloud-based electronic health records and increasing company activities are expected to fuel the growth of the studied segment over the forecast period.
North America is Expected to Have the Significant Market Share Over the Forecast Period
- North America is poised to hold a significant share of the market during the forecast period, mainly due to various factors such as the increasing adoption of healthcare IT solutions related to technological advancements, rising awareness of insurance policies, and the growing utilization of provider network management systems and solutions. Additionally, the region's market growth is expected to be fueled by factors such as the rising awareness of electronic health records (EHRs), the high utilization of healthcare IT solutions, and the growing elderly population.
- The increasing healthcare expenditure in the region is expected to boost market growth by driving the adoption of technologically advanced software and solutions that automate various healthcare payer processes, leading to savings in time and costs compared to traditional manual procedures. According to the Centers for Medicare & Medicaid Services (CMS) 2021 data, the National Health Expenditure (NHE) increased by 2.7% to USD 4.3 trillion (USD 12,914 per person), which accounted for 18.3% of GDP. Private health insurance spending also increased by 5.8% to USD 1.2 trillion in 2021. Other third-party payers and programs and public health activity were USD 596.6 billion in 2021, and hospital expenditures grew by 4.4% to USD 1.3 trillion in 2021.
- Moreover, the rising trend of companies adopting various business strategies, such as collaboration and partnership, is also contributing to market growth in the region during the forecast period. For instance, in December 2021, Stonebrook Risk Solutions partnered with Mphasis to develop a disruptive digital platform that transforms healthcare across the United States. The platform connects regional health plans, insurance companies, pharmacy benefits, consumer-directed health programs, and medical management companies into a nationwide network of providers.
- Additionally, the increasing number of products, software, and solutions launched in the region is also contributing to market growth. For example, in June 2021, McKesson Canada launched the most comprehensive set of integrated digital solutions in Canada, designed to improve specialty physicians' capacity to support their patients across their entire healthcare journey. This program builds on continuing efforts to improve Canadians' digital offerings. Given these factors, the market is expected to grow significantly during the forecast period.
Healthcare Provider Network Management Industry Overview
The healthcare provider network management market is consolidated, with a few key companies dominating the market. The key players are adopting different growth strategies to enhance their market presence, such as partnerships, agreements, collaborations, new product launches, geographical expansions, mergers, and acquisitions. Optum, Inc., Change Healthcare, Infosys Limited, McKesson Corporation, and Mphasis Limited are among the major players in the market.
Healthcare Provider Network Management Market Leaders
-
Infosys Limited
-
Mckesson Corporation
-
Optum, Inc.
-
Change Healthcare
-
Mphasis Limited
*Disclaimer: Major Players sorted in no particular order
Healthcare Provider Network Management Market News
- January 2023: Great Speech announced a strategic partnership with Health Network One to expand their specialized speech therapy services to over 5 million members across the nation. This collaboration is expected to enhance the payer's specialty network management solutions in the country.
- December 2022: Prime Health Services acquired the InterGroup provider network, which includes a comprehensive PPO network for auto, workers' compensation, and group health. This acquisition is set to bolster Prime Health Services' provider network in the Mid-Atlantic region, covering states such as Pennsylvania, New Jersey, Delaware, and West Virginia.
Table of Contents
1. INTRODUCTION
- 1.1 Study Assumptions and Market Definition
- 1.2 Scope of the Study
2. RESEARCH METHODOLOGY
3. EXECUTIVE SUMMARY
4. MARKET DYNAMICS
- 4.1 Market Overview
-
4.2 Market Drivers
- 4.2.1 Rising Quality of Care by Using Payer Reporting Requirements
- 4.2.2 Technological Advancements related to Healthcare IT Solutions
- 4.2.3 Rising Awareness about Insurance Policies
-
4.3 Market Restraints
- 4.3.1 High Cost of Installation and Maintenance of Software
- 4.3.2 Data Security Issues and Cyberattacks
-
4.4 Porter's Five Forces Analysis
- 4.4.1 Threat of New Entrants
- 4.4.2 Bargaining Power of Buyers/Consumers
- 4.4.3 Bargaining Power of Suppliers
- 4.4.4 Threat of Substitute Products
- 4.4.5 Intensity of Competitive Rivalry
5. MARKET SEGMENTATION (Market Size by Value - USD million)
-
5.1 By Component
- 5.1.1 Software/Platforms
- 5.1.2 Services
-
5.2 By Delivery Mode
- 5.2.1 On-premise Delivery
- 5.2.2 Cloud-based Delivery
-
5.3 By End User
- 5.3.1 Payers
- 5.3.2 Private Health Insurance
- 5.3.3 Public Health Insurance
-
5.4 Geography
- 5.4.1 North America
- 5.4.1.1 United States
- 5.4.1.2 Canada
- 5.4.1.3 Mexico
- 5.4.2 Europe
- 5.4.2.1 Germany
- 5.4.2.2 United Kingdom
- 5.4.2.3 France
- 5.4.2.4 Italy
- 5.4.2.5 Spain
- 5.4.2.6 Rest of Europe
- 5.4.3 Asia-Pacific
- 5.4.3.1 China
- 5.4.3.2 Japan
- 5.4.3.3 India
- 5.4.3.4 Australia
- 5.4.3.5 South Korea
- 5.4.3.6 Rest of Asia-Pacific
- 5.4.4 Middle East and Africa
- 5.4.4.1 GCC
- 5.4.4.2 South Africa
- 5.4.4.3 Rest of Middle East and Africa
- 5.4.5 South America
- 5.4.5.1 Brazil
- 5.4.5.2 Argentina
- 5.4.5.3 Rest of South America
6. COMPETITIVE LANDSCAPE
-
6.1 Company Profiles
- 6.1.1 Change Healthcare
- 6.1.2 Infosys Limited
- 6.1.3 Appian
- 6.1.4 Optum, Inc.
- 6.1.5 Artivatic AI
- 6.1.6 Centene Corporation (Envolve Health)
- 6.1.7 RELX Group (LexisNexis Risk Solutions)
- 6.1.8 Skygen USA, LLC,
- 6.1.9 Atos SE (Syntel, Inc.)
- 6.1.10 Mphasis Limited
- 6.1.11 OSPLabs
- 6.1.12 McKesson Corporation
- 6.1.13 Virtusa Corporation
- *List Not Exhaustive
7. MARKET OPPORTUNITIES AND FUTURE TRENDS
** Subject To AvailablityHealthcare Provider Network Management Industry Segmentation
As per the scope of the report, provider network management solutions gather data from various healthcare ecosystems to improve operational efficiencies. These data management systems can offer a single point of access to data from throughout a healthcare organization, including fee schedules, health plans, regulatory compliance, and workflows, as well as send secure alerts to patients as necessary, such as appointment reminders or confirmation of claim statuses to the patients. These systems are used to consolidate patients' data, including care plans, lab results, authorizations, and medical claims.
The healthcare provider network management market is segmented by component (software/platforms and services), delivery mode (on-premise delivery and cloud-based delivery), end user (payers, private health insurance, and public health insurance), and geography (North America, Europe, Asia-Pacific, Middle East and Africa, and South America). The market report also covers the estimated sizes and trends for 17 different countries across major regions globally.
The report offers the value (in USD) for the above segments.
| By Component | Software/Platforms | |
| Services | ||
| By Delivery Mode | On-premise Delivery | |
| Cloud-based Delivery | ||
| By End User | Payers | |
| Private Health Insurance | ||
| Public Health Insurance | ||
| Geography | North America | United States |
| Canada | ||
| Mexico | ||
| Geography | Europe | Germany |
| United Kingdom | ||
| France | ||
| Italy | ||
| Spain | ||
| Rest of Europe | ||
| Geography | Asia-Pacific | China |
| Japan | ||
| India | ||
| Australia | ||
| South Korea | ||
| Rest of Asia-Pacific | ||
| Geography | Middle East and Africa | GCC |
| South Africa | ||
| Rest of Middle East and Africa | ||
| Geography | South America | Brazil |
| Argentina | ||
| Rest of South America |
Frequently Asked Questions
What is the current Healthcare Provider Network Management Market size?
The Healthcare Provider Network Management Market is projected to register a CAGR of 15.5% during the forecast period (2024-2029)
Who are the key players in Healthcare Provider Network Management Market?
Infosys Limited, Mckesson Corporation, Optum, Inc., Change Healthcare and Mphasis Limited are the major companies operating in the Healthcare Provider Network Management Market.
Which is the fastest growing region in Healthcare Provider Network Management Market?
Asia Pacific is estimated to grow at the highest CAGR over the forecast period (2024-2029).
Which region has the biggest share in Healthcare Provider Network Management Market?
In 2024, the North America accounts for the largest market share in Healthcare Provider Network Management Market.
What years does this Healthcare Provider Network Management Market cover?
The report covers the Healthcare Provider Network Management Market historical market size for years: 2020, 2021, 2022 and 2023. The report also forecasts the Healthcare Provider Network Management Market size for years: 2024, 2025, 2026, 2027, 2028 and 2029.
Healthcare Provider Network Management Industry Report
Statistics for the 2024 Healthcare Provider Network Management market share, size and revenue growth rate, created by Mordor Intelligence™ Industry Reports. Healthcare Provider Network Management analysis includes a market forecast outlook to for 2024 to 2029 and historical overview. Get a sample of this industry analysis as a free report PDF download.