Market Size of Healthcare Provider Network Management Industry
| Study Period | 2020 - 2029 |
| Base Year For Estimation | 2023 |
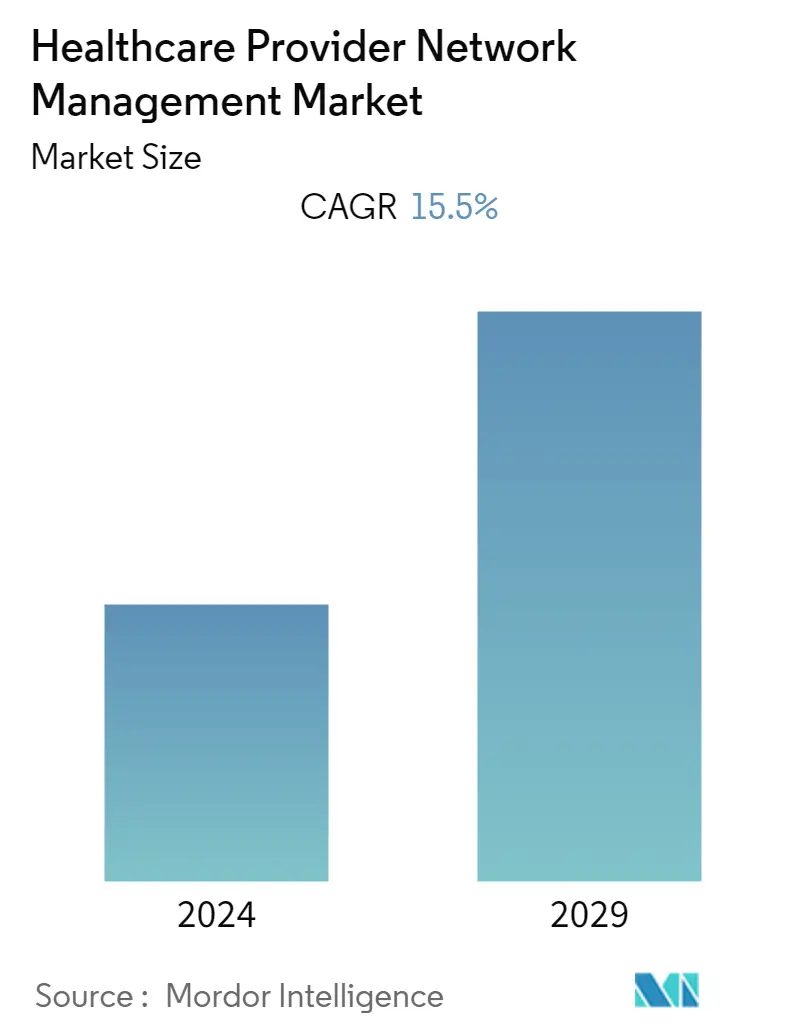
| CAGR | 15.50 % |
| Fastest Growing Market | Asia Pacific |
| Largest Market | North America |
| Market Concentration | High |
Major Players
*Disclaimer: Major Players sorted in no particular order |
Healthcare Provider Network Management Market Analysis
- The healthcare provider network management market is expected to witness a CAGR of 15.5% over the forecast period.
- The COVID-19 pandemic significantly impacted market growth, particularly in the healthcare sector. Healthcare provider management solutions have emerged as a useful tool in automating various processes, thus saving time and expenses. For example, a National Academy of Medicine (NAM) Perspectives article reported that healthcare insurance providers adopted a provider network management solution due to the increase in operating expenses resulting from the growing volume of COVID-19 patients and deferred health services. This solution helped manage claims with greater accuracy of provider networks, lower costs, and less burden on providers. As healthcare providers increasingly adopt provider network management solutions, the market has seen significant growth and is expected to continue growing over the forecast period.
- Several factors are expected to boost market growth, such as the rising quality of care through payer reporting requirements, increasing technological advancements related to healthcare IT solutions, and growing awareness about insurance policies. The rising number of people using insurance to deal with medical costs, such as treatment, hospitalization, and health check-ups, further fuels the demand for provider network management payer services, which is anticipated to drive market growth.
- The India Brand Equity Foundation (IBEF) published its Insurance Industry Report in November 2022, which showed an increase in the number of people who purchased insurance policies. The gross first-year premiums of life insurers increased by 6.94%, totaling INR 2,27,188 crore (USD 29.54 billion) in 2021-2022 (until 31st January 2022). The report also indicated that the new business premiums of life insurers had increased by 88.64% to INR 24,480.36 crore (USD 3.12 billion) in May 2021.
- Additionally, the emergence of technologically advanced solutions and systems in healthcare IT is expected to increase the adoption of provider network management solutions, thereby bolstering market growth. For example, TidalHealth partnered with Regard, an artificial intelligence (AI) software startup, in August 2022 to improve patient diagnostic accuracy, minimize physician exhaustion, and increase income through improved documentation. Modulim launched a software solution in November 2022 designed to empower clinicians with remote access to data insights and scalability to enhance clinical workflow across enterprises.
- Digital technologies also aid in the skillful management of large amounts of data, encourage value addition to the organization, and streamline compliance activities, assisting businesses in avoiding unintended, unanticipated outcomes. By using technology for data integration, analytics, and visualization, compliance activities are being digitized to enhance comprehension. It also helps prevent adverse events by employing robotic process automation and other cognitive technologies such as machine learning and artificial intelligence. These benefits are expected to increase the adoption of provider network management systems and platforms, propelling the market growth.
- Furthermore, the increasing company activities in developing advanced software and solutions are contributing to market growth. Optum launched Optum Specialty Fusion, a specialty medication management solution, in February 2022 to simplify care for patients with complex conditions and lower the cost of expensive specialty drugs.
- Specialized Fusion offers payers and providers real-time healthcare insight into the most efficient specialty treatments at the patient's lowest cost using Optum's data and clinical experience. Innovaccer launched Provider Network Management Solutions in March 2021 to assist healthcare payers in accessing a complete view and exercising control over their provider network performance. The solution creates a unified pool of accurate provider data, determines effective methods, incentivizes providers, and streamlines communication.
- Despite the expected growth of the studied market, some factors may impede market growth over the forecast period. The high cost of software installation and maintenance, as well as data security issues and cyberattacks, are likely to be barriers.
Healthcare Provider Network Management Industry Segmentation
As per the scope of the report, provider network management solutions gather data from various healthcare ecosystems to improve operational efficiencies. These data management systems can offer a single point of access to data from throughout a healthcare organization, including fee schedules, health plans, regulatory compliance, and workflows, as well as send secure alerts to patients as necessary, such as appointment reminders or confirmation of claim statuses to the patients. These systems are used to consolidate patients' data, including care plans, lab results, authorizations, and medical claims.
The healthcare provider network management market is segmented by component (software/platforms and services), delivery mode (on-premise delivery and cloud-based delivery), end user (payers, private health insurance, and public health insurance), and geography (North America, Europe, Asia-Pacific, Middle East and Africa, and South America). The market report also covers the estimated sizes and trends for 17 different countries across major regions globally.
The report offers the value (in USD) for the above segments.
| By Component | |
| Software/Platforms | |
| Services |
| By Delivery Mode | |
| On-premise Delivery | |
| Cloud-based Delivery |
| By End User | |
| Payers | |
| Private Health Insurance | |
| Public Health Insurance |
| Geography | ||||||||
| ||||||||
| ||||||||
| ||||||||
| ||||||||
|
Healthcare Provider Network Management Market Size Summary
The healthcare provider network management market is poised for substantial growth, driven by the increasing adoption of automated solutions that streamline processes and reduce costs. The COVID-19 pandemic has accelerated the need for these solutions, as healthcare providers sought to manage the surge in patients and deferred services more efficiently. Technological advancements in healthcare IT, coupled with rising awareness of insurance policies, are further propelling market expansion. The demand for provider network management services is bolstered by the growing number of individuals utilizing insurance to cover medical expenses, which underscores the importance of efficient network management in delivering quality care.
The market is also witnessing a shift towards cloud-based delivery modes, offering cost-effective and scalable solutions for healthcare providers. The integration of advanced technologies, such as artificial intelligence and data analytics, is enhancing the capabilities of provider network management systems, facilitating better data management and compliance. North America is expected to maintain a significant market share, supported by high healthcare expenditure and the adoption of electronic health records. The region's growth is further fueled by strategic collaborations and the introduction of innovative software solutions. Despite potential challenges like high implementation costs and data security concerns, the market is set to experience robust growth, driven by the efforts of key players and the ongoing digital transformation in healthcare.
Healthcare Provider Network Management Market Size - Table of Contents
-
1. MARKET DYNAMICS
-
1.1 Market Overview
-
1.2 Market Drivers
-
1.2.1 Rising Quality of Care by Using Payer Reporting Requirements
-
1.2.2 Technological Advancements related to Healthcare IT Solutions
-
1.2.3 Rising Awareness about Insurance Policies
-
-
1.3 Market Restraints
-
1.3.1 High Cost of Installation and Maintenance of Software
-
1.3.2 Data Security Issues and Cyberattacks
-
-
1.4 Porter's Five Forces Analysis
-
1.4.1 Threat of New Entrants
-
1.4.2 Bargaining Power of Buyers/Consumers
-
1.4.3 Bargaining Power of Suppliers
-
1.4.4 Threat of Substitute Products
-
1.4.5 Intensity of Competitive Rivalry
-
-
-
2. MARKET SEGMENTATION (Market Size by Value - USD million)
-
2.1 By Component
-
2.1.1 Software/Platforms
-
2.1.2 Services
-
-
2.2 By Delivery Mode
-
2.2.1 On-premise Delivery
-
2.2.2 Cloud-based Delivery
-
-
2.3 By End User
-
2.3.1 Payers
-
2.3.2 Private Health Insurance
-
2.3.3 Public Health Insurance
-
-
2.4 Geography
-
2.4.1 North America
-
2.4.1.1 United States
-
2.4.1.2 Canada
-
2.4.1.3 Mexico
-
-
2.4.2 Europe
-
2.4.2.1 Germany
-
2.4.2.2 United Kingdom
-
2.4.2.3 France
-
2.4.2.4 Italy
-
2.4.2.5 Spain
-
2.4.2.6 Rest of Europe
-
-
2.4.3 Asia-Pacific
-
2.4.3.1 China
-
2.4.3.2 Japan
-
2.4.3.3 India
-
2.4.3.4 Australia
-
2.4.3.5 South Korea
-
2.4.3.6 Rest of Asia-Pacific
-
-
2.4.4 Middle East and Africa
-
2.4.4.1 GCC
-
2.4.4.2 South Africa
-
2.4.4.3 Rest of Middle East and Africa
-
-
2.4.5 South America
-
2.4.5.1 Brazil
-
2.4.5.2 Argentina
-
2.4.5.3 Rest of South America
-
-
-
Healthcare Provider Network Management Market Size FAQs
What is the current Healthcare Provider Network Management Market size?
The Healthcare Provider Network Management Market is projected to register a CAGR of 15.5% during the forecast period (2024-2029)
Who are the key players in Healthcare Provider Network Management Market?
Infosys Limited, Mckesson Corporation, Optum, Inc., Change Healthcare and Mphasis Limited are the major companies operating in the Healthcare Provider Network Management Market.

