US Healthcare BPO Market Size
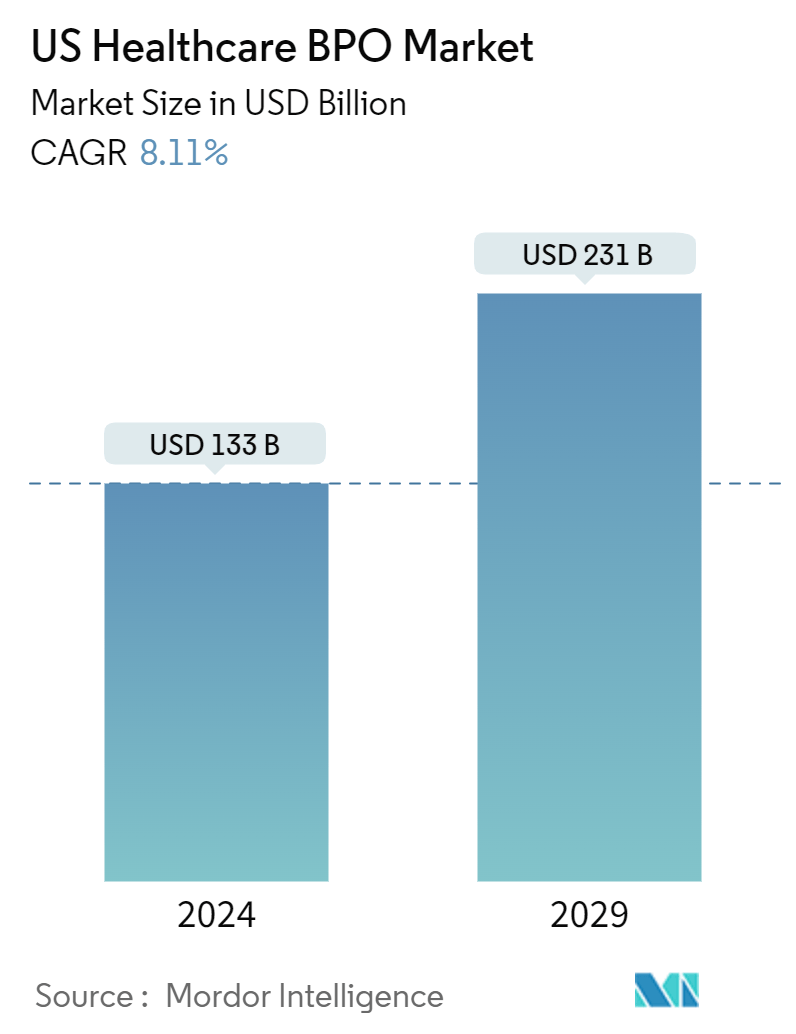
| Study Period | 2019 - 2029 |
| Base Year For Estimation | 2023 |
| Market Size (2024) | USD 133 Billion |
| Market Size (2029) | USD 231 Billion |
| CAGR (2024 - 2029) | 8.11 % |
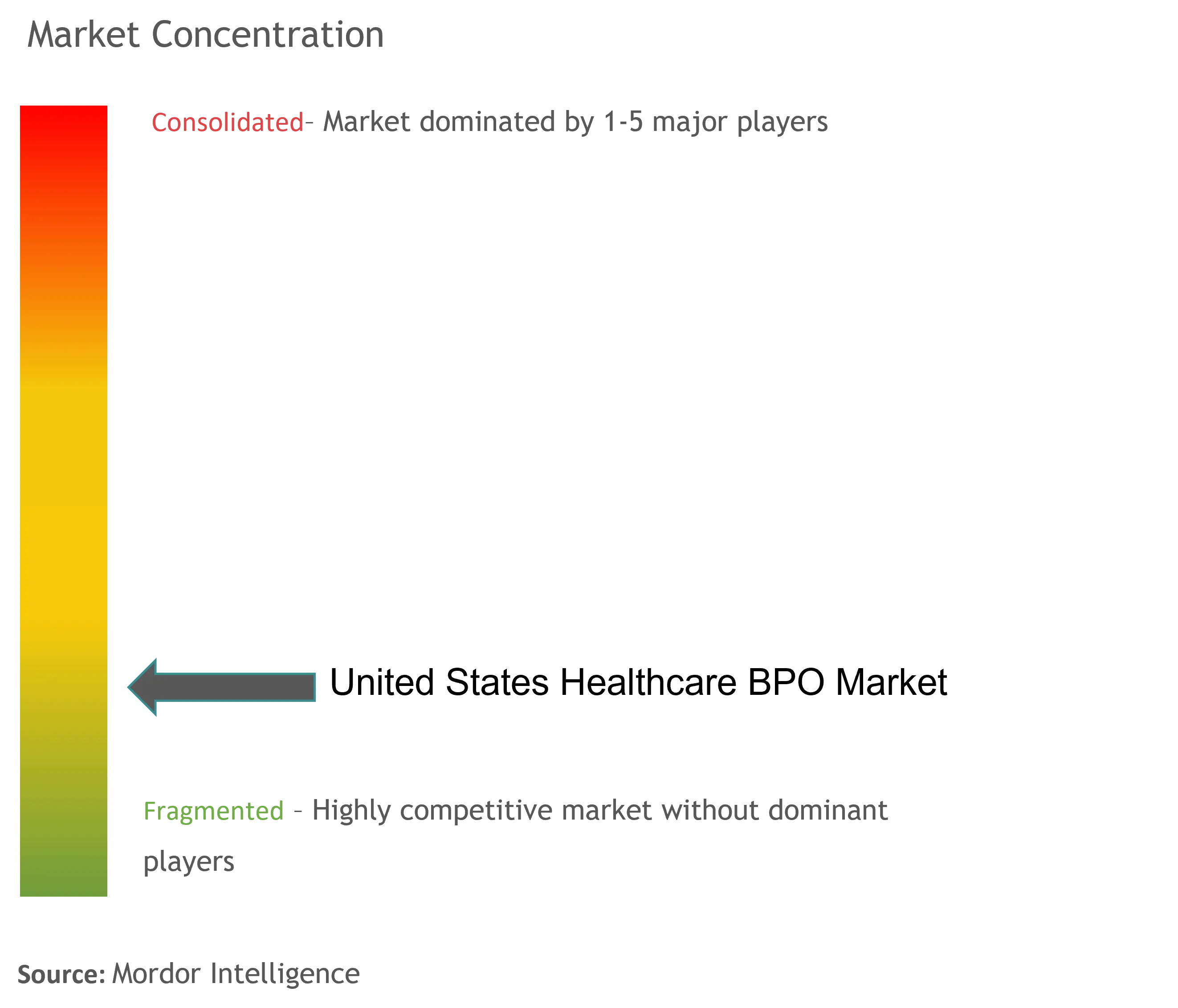
| Market Concentration | Low |
Major Players
*Disclaimer: Major Players sorted in no particular order |
US Healthcare BPO Market Analysis
The US Healthcare BPO Market size is estimated at USD 133 billion in 2024, and is expected to reach USD 231 billion by 2029, growing at a CAGR of 8.11% during the forecast period (2024-2029).
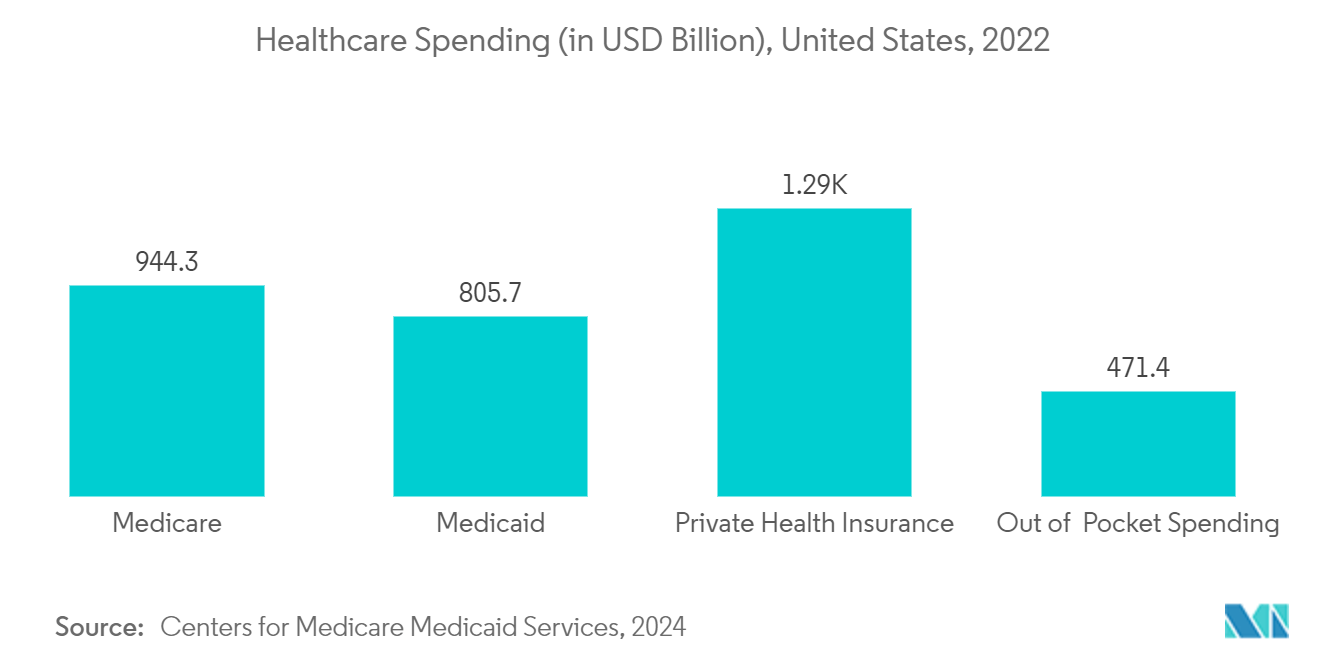
The US healthcare system favors new opportunities and growth due to the quick adoption of advanced technologies among pharmacies, pharmaceutical companies, medical equipment manufacturers, and medical care facilities. The infrastructure of this industry depends on specialized professionals who manage the operations. The expansion of the US healthcare BPO market can be attributed to the heightened awareness of outsourcing healthcare IT services and the significant presence of leading market players in the country.
Another key driving factor is the increasing strategic actions of leading firms, including product launches, alliances, and other actions, which are expected to drive market expansion throughout the forecast period. For example, in December 2023, Acquire BPO expanded its geographical presence in Texas, United States, to address the increasing demand for outsourcing solutions. The opening of the Irving headquarters reinforces the company's position as a significant player in the US market, enabling improved collaborations with clients. In March 2022, CPSI, a company specializing in healthcare solutions, acquired Healthcare Resource Group Inc. in Spokane, Washington. HRG is a prominent provider of tailored revenue cycle management (RCM) solutions and consulting services that help hospitals and clinics enhance efficiency, profitability, and patient satisfaction.
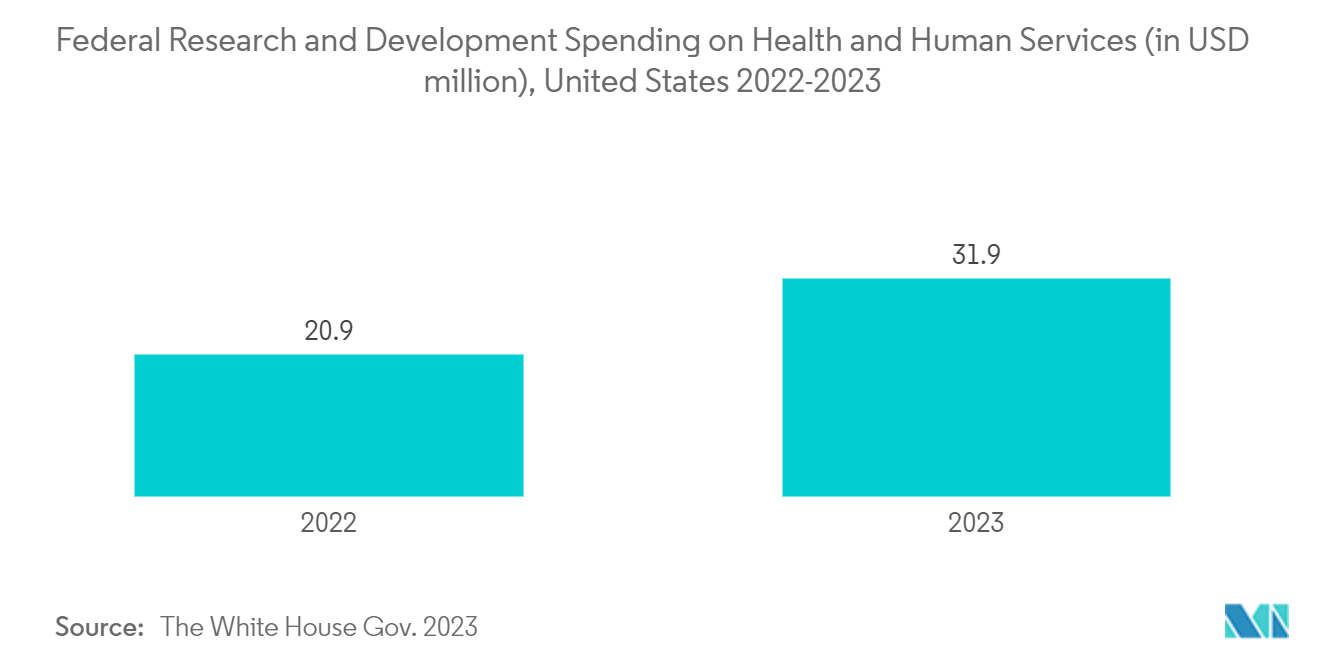
The increase in government initiatives within the country is expected to propel market growth. For instance, in February 2022, the Department of Health and Human Services (HHS) allocated nearly USD 55 million to 29 health centers funded by the HRSA to enhance healthcare access and quality for underserved populations via virtual care. Virtual care has significantly transformed the patient experience, particularly during the COVID-19 pandemic. Thus, initiatives by government organizations are anticipated to propel market growth across the country.
Moreover, the rising demand for insurance, the need to reduce healthcare delivery expenses, the consolidation of the healthcare system, pharmaceutical companies encountering patent expirations, and the compulsory adoption of ICD-10 codes (the 10th revision of the International Statistical Classification of Diseases and Related Health Problems) are significant drivers behind the expansion of the healthcare BPO market in the United States.
Thus, the market is expected to grow in the United States due to the abovementioned factors, including various government initiatives and strategic actions by market players. However, data integrity and confidentiality may restrain market growth.
US Healthcare BPO Market Trends
The Claims Management Segment is Expected to Have the Highest CAGR Over the Forecast Period
Claims processing outsourcing (CPO) is a relatively new business concept for insurance firms. It has emerged as the preferred option for organizations aiming to minimize operating expenses while improving service quality. Understanding the relationship between policyholders, healthcare providers, and insurance companies is essential for understanding the details of the medical billing and coding process.
Medical claims management is the process of billing, filling, updating, and processing medical claims related to a patient's diagnosis, treatments, and medications. Many hospitals and medical facilities outsource these tasks to medical claims management firms, as maintaining patient records, interacting with health insurance agencies, and preparing medical service invoices are time-consuming processes.
The rising burden of chronic diseases, the aging population, and the rising healthcare claims are driving the segment's expansion. For instance, according to the data published by the American Cancer Society in January 2024, an estimated 2.0 million new cancer cases will be diagnosed in the United States in 2024, among which prostate cancer is estimated to be the highest with 299,010 cases, followed by 234,580 cases of lung cancer, and 313,510 cases of female breast cancer. Therefore, with the rising burden of chronic diseases such as cancer, insurance companies can receive more claims from healthcare providers to offset the treatment cost incurred for cancer, which drives the demand for claim management services, thereby boosting the segment's growth.
Strategic activities by market players, such as partnerships, are expected to boost market growth over the forecast period. For instance, in May 2024, Aflac established a strategic collaboration with Nayya to transform how employees utilize their supplemental health benefits. Nayya will facilitate the integration of supplemental health claims for employers within Aflac’s top-tier group benefits sector, streamlining the claims filing process and minimizing the associated complexities and time.
In March 2024, UnitedHealth Group mentioned that its subsidiary Change Healthcare completely rebuilt and restored its cloud-based services for managing medical claims. Change's Assurance and Relay Exchange are cloud-based applications that depend on authentication services. Assurance is a software solution for managing medical claims and remittances, whereas Relay Exchange is a clearinghouse that verifies insurance claims for inaccuracies. Thus, such initiatives by market players are anticipated to drive the segment's growth in the United States.
Thus, all the factors above, such as the growing burden of chronic diseases and strategic activities by the market players, are expected to boost the segment's growth.
The Revenue Cycle Management Segment is Expected to Hold a Significant Share Over the Forecast Period
Revenue cycle management (RCM) is a tool healthcare institutions use to monitor all financial interactions with patients, from their first appointment until the settlement of any outstanding debt. All clinical and administrative tasks involved in managing and collecting patient service revenues collectively come under RCM. Therefore, the growing need for RCM services in healthcare is anticipated to promote the segment's expansion.
RCM provides various advantages to the supplier, from billing and collections to administrative responsibilities. It is a cutting-edge system that manages administrative tasks via sophisticated billing, payment processing, and electronic health record systems. According to an article published by the Medical Group Management Association (MGMA) in June 2022, medical practices that outsource their RCM experience increased performance in collections, staff efficiency, and other sectors. Thus, owing to the benefits associated with RCM and its growing adoption, the segment is expected to grow over the forecast period.
The market players are focusing on new partnerships and agreements to bolster their market positions, resulting in the segment's growth. For instance, in July 2022, Waystar, a revenue cycle management (RCM) vendor, planned to buy Patientco in the latest transaction involving an RCM vendor and a patient payment company.
The RCM vendor hopes that the combination will improve patients' financial experience by providing user-friendly options for medical costs. In December 2022, Luminis Health, situated in Annapolis, Maryland, selected VisiQuate, an AI-powered analytics firm, to handle its revenue cycle management operations. Similarly, in November 2022, Cornerstone Specialty Hospitals partnered with CareCloud to take on its revenue cycle management services in West Monroe, Louisiana.
Thus, the factors mentioned above, such as the enormous benefits of RCM outsourcing and strategic collaborations between healthcare companies and market vendors, are expected to boost the segment's growth.
US Healthcare BPO Industry Overview
The US healthcare BPO market is fragmented. It consists of several big and small-scale players. The competitive landscape includes an analysis of a few international and local companies that hold significant market shares and are well known. Some of the major players in the market studied are Accenture PLC, OutsourceRCM, Genpact Limited, IBM Corporation, Parexel International, and Cognizant.
US Healthcare BPO Market Leaders
*Disclaimer: Major Players sorted in no particular order
US Healthcare BPO Market News
- August 2024: EnableComp, a provider of specialty revenue cycle solutions for the healthcare sector, completed the acquisition of ANI Healthcare Solutions, a denial management company based in San Francisco. This acquisition allows EnableComp to enhance its comprehensive portfolio by incorporating ANI's expertise in denial management while augmenting the capabilities of the E360 RCM intelligent automation platform.
- July 2024: Everise established a strategic partnership with Sanas, a global pioneer in real-time speech and accent transformation technology. This collaboration grants Everise exclusive access to utilize Sanas’ services within the healthcare business process outsourcing (BPO) sector. This is aimed at boosting customer satisfaction, improving productivity, and increasing cost efficiencies in this competitive field.
US Healthcare BPO Market Report - Table of Contents
1. INTRODUCTION
- 1.1 Study Assumptions and Market Definition
- 1.2 Scope of the Study
2. RESEARCH METHODOLOGY
3. EXECUTIVE SUMMARY
4. MARKET DYNAMICS
- 4.1 Market Overview
-
4.2 Market Drivers
- 4.2.1 Rapid Increase in Clinical Process Outsourcing (CPO)
- 4.2.2 Increasing R&D in the Healthcare Industry
-
4.3 Market Restraints
- 4.3.1 Data Integrity and Confidentiality
-
4.4 Porter's Five Forces Analysis
- 4.4.1 Threat of New Entrants
- 4.4.2 Bargaining Power of Buyers/Consumers
- 4.4.3 Bargaining Power of Suppliers
- 4.4.4 Threat of Substitute Products
- 4.4.5 Intensity of Competitive Rivalry
5. MARKET SEGMENTATION (Market Size by Value - USD)
-
5.1 By Payer Service
- 5.1.1 Human Resource Management
- 5.1.2 Claims Management
- 5.1.3 Customer Relationship Management (CRM)
- 5.1.4 Operational/Administrative Management
- 5.1.5 Care Management
- 5.1.6 Provider Management
- 5.1.7 Other Payer Services
-
5.2 By Provider Service
- 5.2.1 Patient Enrollment and Strategic Planning
- 5.2.2 Patient Care Service
- 5.2.3 Revenue Cycle Management
-
5.3 By Pharmaceutical Service
- 5.3.1 Research and Development
- 5.3.2 Manufacturing
- 5.3.3 Non-clinical Services
- 5.3.3.1 Supply Chain Management and Logistics
- 5.3.3.2 Sales and Marketing Services
- 5.3.3.3 Other Non-clinical Services
6. COMPETITIVE LANDSCAPE
-
6.1 Company Profiles
- 6.1.1 Accenture PLC
- 6.1.2 Capgemini
- 6.1.3 Cognizant
- 6.1.4 GeBBs Healthcare Solutions
- 6.1.5 Genpact Limited
- 6.1.6 IBM Corporation
- 6.1.7 IQVIA
- 6.1.8 Parexel International
- 6.1.9 Sutherland Healthcare Solutions
- 6.1.10 UnitedHealth Group Incorporated
- 6.1.11 OutsourceRCM
- *List Not Exhaustive
7. MARKET OPPORTUNITIES AND FUTURE TRENDS
** Subject To AvailablityUS Healthcare BPO Industry Analysis
Healthcare BPO (business process outsourcing) refers to a process in which healthcare providers select the most suited third-party vendors for specific business processes. This allows hospitals and medical professionals to spend their energy and valuable time on patient care.
As per the scope of the report, the US healthcare BPO market is segmented by payer service, provider service, and pharmaceutical service. By payer service, the market is segmented into human resource management, claims management, customer relationship management (CRM), operational/administrative management, care management, provider management, and other payer services. By provider service, the market is segmented into patient enrollment and strategic planning, patient care service, and revenue cycle management. By pharmaceutical service, the market is segmented into research and development, manufacturing, and non-clinical service). For each segment, the market size is provided in terms of value in USD.
| By Payer Service | Human Resource Management | |
| Claims Management | ||
| Customer Relationship Management (CRM) | ||
| Operational/Administrative Management | ||
| Care Management | ||
| Provider Management | ||
| Other Payer Services | ||
| By Provider Service | Patient Enrollment and Strategic Planning | |
| Patient Care Service | ||
| Revenue Cycle Management | ||
| By Pharmaceutical Service | Research and Development | |
| Manufacturing | ||
| Non-clinical Services | Supply Chain Management and Logistics | |
| Sales and Marketing Services | ||
| Other Non-clinical Services |
US Healthcare BPO Market Research FAQs
How big is the US Healthcare BPO Market?
The US Healthcare BPO Market size is expected to reach USD 133 billion in 2024 and grow at a CAGR of 8.11% to reach USD 231 billion by 2029.
What is the current US Healthcare BPO Market size?
In 2024, the US Healthcare BPO Market size is expected to reach USD 133 billion.
Who are the key players in US Healthcare BPO Market?
Accenture PLC, Genpact Limited, Parexel International, Cognizant and OutsourceRCM are the major companies operating in the US Healthcare BPO Market.
What years does this US Healthcare BPO Market cover, and what was the market size in 2023?
In 2023, the US Healthcare BPO Market size was estimated at USD 122.21 billion. The report covers the US Healthcare BPO Market historical market size for years: 2019, 2020, 2021, 2022 and 2023. The report also forecasts the US Healthcare BPO Market size for years: 2024, 2025, 2026, 2027, 2028 and 2029.
US Healthcare BPO Industry Report
Statistics for the 2024 US Healthcare BPO market share, size and revenue growth rate, created by Mordor Intelligence™ Industry Reports. US Healthcare BPO analysis includes a market forecast outlook to 2029 and historical overview. Get a sample of this industry analysis as a free report PDF download.